Risks of Ionizing Radiation
Low Levels of Ionizing Radiation May Cause Harm From The National Academies of Sciences + Engineering + Medicine
All Levels of Radiation Confirmed to Cause Cancer Nuclear Information and Resource Service
Beir VII Report Raises Major Issues for Radiation Protection
Death By Medicine takes a hard examination at the dominant medical paradigm contributing to America's health crisis. Based on Gary Null's ground breaking book on the hundreds of thousands of injuries and deaths caused by conventional medicine, the documentary looks at the medical industrial complex, the pharmaceutical industry's usurpation of the nation's medical schools, research, falsified drug clinical trials, peer reviewed scientific journals, and the complicity of federal health agencies to permit this to happen.
This video clip is cut from the middle & it's Dr. Samuel Epstein talking about the amount of radiation in a mammogram and cumulative effects. He says each one is 200 times the amount of a chest x-ray and that we approach levels of being 1 mile from the Hiroshima atomic bomb with just two mammograms (2D mammography-2 angles each breast - Europe does one angle). More radiation comes with 3D tomosynthesis mammography, essentially a CT scan of the breast, which is xrays from 25 angles.
The article below is a radiologist appealing to his colleagues to resist the knee-jerk CT scans of today due to the National Academy of Science's report warning that "there is no evidence that any level is safe or beneficial" and that today's patients not uncommonly receiving multiple CT scans are easily approaching the high levels of medical radiation used in the 30's and 40's which resulted in so much horrific damage seen in their later years. He's concerned about a consumer class action suit against radiologists and oncologists if care isn't taken to track and minimize CT use.
Accessing the article requires participating in multiple surveys and a Medscape account so we used our account and copied here for you:
Imaging X-rays Cause Cancer: A Call to Action for Caregivers and Patients
Author: Richard C. Semelka, MD
Posted: 02/13/2006; Updated: 02/16/2007
This article is a follow-up to one that I had developed for Medscape in the past, which was entitled "Radiation Risk From CT Scans: A Call for Patient-Focused Imaging" (http://www.medscape.com/viewarticle/496297).
That article was the 5th most read article on Medscape in 2005, and the most read article on Medscape's Radiology site. Clearly, this topic is of high interest. Why the need for a follow-up article?
Two reasons: First, to address a document that has come out since the time I wrote the first piece; in September 2005, the National Academy of Science released their 7th report ("Low Levels of Ionizing Radiation May Cause Harm") on the Biological Effects of Ionizing Radiation (BEIR VII), which should be considered the definitive and indisputable authoritative resource on the subject of radiation risk. Another reason to revisit this issue is to further emphasize safety considerations, which I believe we need to consider as we move forward in our various capacities as patients, radiologists, referring physicians and healthcare providers, third-party payers, and legislators.
The intent of this article is to globally address many of the emails, both pro and con, that I have received on this subject after the publication of the radiation piece in 2005.
CT REMAINS A POWERFUL TOOL, BUT ...
Prior to engaging in any discussion of imaging and radiation risk, the first point to emphasize is that computed tomographic (CT) scanning is a powerful and indispensable diagnostic tool. CT, more than any other imaging modality, has heralded a new age of medical practice based on the ability to visualize the inner workings of the human body.
This new age of medical practice is as follows: The diagnosis that you have been given as a patient, to a very large extent, and possibly completely, has been established on the basis of the imaging study that you received.
That diagnosis, with the proper medical management that has stemmed from that diagnosis, may well have saved your life.
In effect, medical imaging has become the modern physical exam.
As part of my teaching to residents, I tell them that, after 2 weeks of experience in CT scanning, a first-year radiology resident is a better diagnostician than any of the greatest clinicians in the pre-CT era, including Sir William Osler and everyone else; medical imaging is that powerful a tool, and CT has been the modality that has most represented this new diagnostic age.
Furthermore, since its initial use for the clinical evaluation of patients in the late 1970s, CT scanning has continued to evolve. The availability of a 64-plus-row multidetector CT facilitates images of extraordinary anatomical display and detail that can be rendered in perfect 3D models. For this reason, any discussion of radiation risks must also be tempered with the recognition of the benefits of CT scanning and the earnest efforts of well-meaning scientists, referring clinicians, and radiologists to improve information that the modality generates, which ultimately is intended to benefit patients.
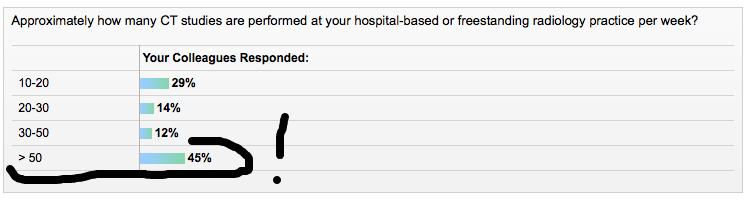
3/25/16 downtown Portland, Oregon area clinics according to Medscape's poll
IMAGING AND CANCER: KIDS MOST IN PERIL
The above being said, the indisputable fact, and in my opinion rendered truly indisputable by the BEIR VII report, is that medical x-rays cause cancer.[1] BEIR VII also emphasizes that there may be no safe lower limit.[1] This statement taken as said has the potential to cause considerable alarm, so my intuitive modification is that perhaps below the dose of a standard body CT, which is approximately 10 mSieverts (mSv; units that radiation dose is measured in), there is likely negligible if any risk for an individual test.
However, even 1 body CT scan (1 CT scan of only 1 of the following regions: the chest region, the abdominal region, or the pelvic region) carries with it some element of risk. The risk that BEIR VII reports is 1 in 1000 chance of developing cancer from a 10 mSv radiation dose. In my prior report, I described what is written on the US Food and Drug Administration Web site, which is a 1 chance in 2000 of developing cancer from a dose of 10 mSv. The BEIR VII report doubles that risk. The risk in children is even higher, with a reported chance of 1 in 550 of developing cancer.[2,3] The following is a table of the standard reported dose of radiation for various common imaging procedures:
Table: Average Radiation Doses Associated With Common Imaging Studies
Risk escalates with multiphase acquisition in a single CT study, and with multiple individual CT tests. Because of their multiphase nature, careful limited use of multiphase renal CT studies and liver CT studies should be considered.
3/25/16 particpated in this poll to access the article.
WHY PATIENTS ARE THE LAST TO KNOW
Another critical aspect of risk is this question: What kind of cancers (malignancies) are triggered by imaging radiation, and when do they occur? As preface to this, the answer in part explains why this information is not generally being conveyed, to date, to patients prior to their undergoing a CT study.
First, the cancers are relatively common in the general population, which means that it is difficult to sort out which cancers have occurred as a direct result from x-rays (unlike, for example, mesothelioma, which is an extremely rare cancer, and therefore its association with asbestos exposure was relatively easy to ascertain); second, the latency period between exposure to x-rays and development of cancer may be extremely long, up to 20 years, which means that the association may be difficult both to deduce and to prove. BEIR VII (and other sources) reported that the malignancies most associated with x-ray exposure are leukemia, thyroid, and breast cancers.[1] The latency period between exposure and development of malignancy they report as 2-5 years for leukemias (and other blood line tumors) and 10-20 years for solid tumors (sarcoma, breast cancers).
Twenty years is a long time -- after 20 years generally the ordering physician or nurse is gone, the radiologist is gone, and the only one left is the patient, who received x-ray radiation as a child and now harbors a malignancy in middle age.
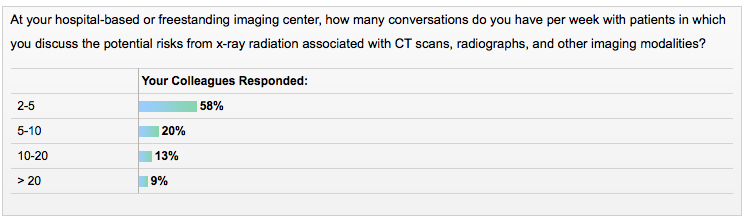
3/25/16 particpated in this poll to access the article.
RADIOLOGY AND RADIATION: THE GATHERING STORM
Explanations as to what has happened to the present time are, I believe, as follows: economic imperatives, and a lack of clear, concrete data that relates specifically to modern x-ray exposure. On the basis of this latter point, the desire of the general radiology community is not to create alarm if the information is not certain. How do we explain the opinion of the radiology community that the data of risk of cancer from x-rays is unclear?
First, the majority of the reports that are specifically about the link between x-rays and the development of cancer are old studies,[4,5] and these cancers have arisen at a time when x-ray exposure was uncontrolled and unmeasured, and enormous doses of radiation were delivered (of course those doses may not be out of line with what patients who undergo multiple CT scans are receiving today); second, our perception is generally derived from immediate experiences -- which I term the "science of the immediate experience"; and, third, the most compelling data related to radiation risk and cancer are derived from atomic bomb survivors. On the surface, it is easy to dismiss equating an atomic bomb explosion that instantly kills thousands of people with an innocuous imaging study -- it turns out the correlation is apt, as described below.
Knowledge of all kinds tends to take a cyclical course, whether the topic is the reasons for market collapses in economies, or, in this case, the dangers of x-radiation. In the 1940s, articles were written in major medical journals describing increased malignancies from x-rays -- at that time because radiologists shared the burden of radiation with patients, because of the nature of fluoroscopy. The reports were mainly about radiologists who developed an increased incidence of leukemia. Some 25 years later, scientist ID Bross lamented in a report entitled The Primacy Principle that when industry develops a procedure in which the safety of that procedure is uncertain, the burden of proof should rest with that industry, rather than with the public, that the procedure is safe.[6]
This maxim he termed the primacy principle, and he was referring to x-rays, interestingly, in the pre-CT era. Taking this forward yet another generation, there are a number of reports, risk models, animal experiments, and human series reports that describe the increased risk of cancer from x-ray exposure[7-16] -- these reports are now escalating in number.
Why is it, then, that radiologists are so reticent to accept the dangers of excessive radiation and have not been leading the charge for reform, accountability, and increased dissemination of knowledge? And why have referring healthcare providers, in particular emergency department clinicians, been so apparently unaware, uninformed, or noncommunicative about the risk of these studies to patients?
I recommend that we deal with this growing crisis by first recognizing the key points outlined below:
LARGE X-RAY DOSES
My personal opinion is that many patients today who are receiving multiple CT scans may well be getting at least comparable doses to subjects that have now developed malignancies from x-ray radiation received in the 1930s and '40s. And, similar to those days when the doses were unknown, the dose that patients receive today over a course of years of multiple CT scans is also completely unknown.
THE SCIENCE OF THE IMMEDIATE EXPERIENCE
This may also be termed intuitive science, which is our innate processing of immediate cause and effect. When we took chemistry in high school and university and performed experiments in labs, we mixed 2 chemicals together, and then the product changed color, or heated up, or smoked, or maybe even exploded; however, in any event, the reaction happened more or less right away. Our brains are attuned to the science of the immediate experience, which probably relates back to survival in its basic form.
This science is basically primordial and based on what we actually see - "seeing is believing - hic Rhodos, hic salte - etc."
When we as radiologists perform a CT scan on a patient, the patient lies down on the table, undergoes the scan, gets up and is perfectly fine (unless there has been a contrast reaction or subcutaneous contrast misinjection), and then leaves and waits to hear back from the ordering provider about the results of the study. There is no skin heating, no burning, no skin reddening, and no hair exfoliation, which are features that we are familiar with as representing x-ray overdoses as experienced in the past. So, fundamentally, our primordial brains reject the concept that we are doing harm, because of our appreciation of the science of the immediate experience.
In fact, what I and other MRI experts have focused on in the recent past as indications for patients to undergo MRI rather than CT are cases in which patients have had contrast reactions with CT contrast (an immediate experience) because MR contrast is associated with many fewer reactions. Or we have focused on patients with kidney failure since iodine contrast in CT can result in worsening renal failure, while the MRI contrast medium gadolinium almost never worsens renal failure, which again is an immediate experience. It is difficult to abstract the immediate visual experience to a scientific concept that is somehow intangible, or at least difficult to grasp or fathom, even though dedicated scientists have proven the concept.
A good conceptual framework to use in understanding the x-ray radiation danger issue is the movement of the earth - the earth rotates along its axis at 1000 miles per hour, and moves around the sun at 87,000 miles per hour -- however, my scientific mind of the immediate experience cannot conceive and therefore believe that. The earth travels at 87,000 miles per hour, how is that possible? I don't see things rushing around past me - things are still, nothing is flying around at that speed. Yet scientists and astrophysicists have proven this point. Am I, as a thoughtful radiologist, whose senses tell me nothing is moving, going to dispute that the earth is moving at 87,000 miles per hour?
The answer is no.
Similarly, there is an entire field of radiation research, with journals devoted to that topic and that topic only, that contain articles written by thoughtful scientists that outline the dangers associated with x-ray radiation.[15,16] Am I going to dispute their findings based on no other science than my science of the immediate experience?
The prudent answer is no.
Of course, having said that, in reading the radiation science literature some research is even more alarming than the BEIR VII report.[15-17] And, my belief is that we have to pay careful attention to this literature, and not dismiss the findings of these scientists. However, major policy shifts should probably only be made based on the consensus of the majority of experienced scientists in that field of research. That is what BEIR VII represents, and its findings are in line with all previous large consensus reports dealing with radiation and safety.[18,19] Am I going to dispute what leading scientists report in their field of expertise, if I have no true expertise?
The answer is no.
EQUATING MEDICAL X-RAYS WITH AN ATOMIC BOMB
Much of BEIR VII and other reports devote great portions of their content to the justification of comparing the effects of medical x-rays with radiation received from exposure to an atomic bomb.[1,18,19]
I will abbreviate it briefly and simply. The atomic bomb survivors, who form the basis of many radiation risk estimates, are subjects who were at a considerable distance from the actual explosion, a distance at which they would receive relatively pure gamma radiation. These are not individuals who had large pieces of metal penetrating their bodies, or high radiation dose particles like alpha particles hitting them. These were subjects who received a single exposure of gamma radiation, but in large numbers, so that meaningful and reliable statistics can be generated.
The BEIR VII report looks at the most recent survivor data in these subjects, especially those patients in the low-dose group of less than 100 mSv, which is essentially the range of medical x-ray exposure from CT scans.[1] In that group, the BEIR VII investigators found an increased risk of developing cancer, and they and other reports emphasize that there is no lower threshold (of safety).[1,18,19] Radiation physicists and radiation biologists generally consider the cancer-inducing potential of gamma rays and x-rays to be approximately equivalent, and I (recalling that the earth is traveling at 87,000 miles per hour) do not have the scientific training or experience to dispute that.
One other point that should be mentioned is that one should always hold with some skepticism the information provided by an individual when there is a perceived financial advantage or incentive or conflict of interest, and I have heard that skepticism leveled against these scientists. I cannot conceive how it could possibly be in their financial interest to release a report cautioning against medial x-radiation. I could only conceive that there would be a tremendous financial disincentive to make such a claim.
THE ECONOMICS OF CT SCANNING
I do not wish to delve too much into the financial aspects of decision making on this subject; I hope that economics is not the major stumbling block for the acceptance of judicious use of medical x-rays. It should be clear that CT scanning generates a tremendous amount of money for the healthcare system, not only for radiologists, but for hospitals, equipment manufacturers, and pharmaceutical companies.
Concern that decreasing the number of CT scans would financially jeopardize these institutions should be tempered with the recognition that the concomitant increase in appropriately performed MRI studies would offset any decrease in CT scans.
Ultimately, patient safety and doing what is clinically appropriate for the patient should prevail in all of our minds.
BEIR VII, the definitive report, has been released. BEIR VII states that medical x-rays cause cancer, even in the doses of individual CT scans. From the perspective of a radiologist, I believe that at this time sufficient information is available to prove that radiation doses in the range of CT scans cause cancer. We can no longer justify to ourselves as radiologists and ordering healthcare providers that there is not enough good data to support the link between imaging radiation and cancer. I believe that the burden of proof rests with us, not with our patients. It has been said that in the scientific community of radiation expert scientists there is no dispute about the safety aspects of radiation; it is only in the radiology community that there dwells this uncertainty.
A 4-POINT PLAN TO KEEP OUR PATIENTS SAFE
There are 4 things we must do to safeguard our patients, and these criteria reiterate what I have said in previous articles on this topic on Medscape:
Use CT judiciously.
Reduce the radiation exposure associated with CT scans.
Substitute other imaging modalities that are diagnostically superior or equivalent to CT for various clinical indications. It can also be debated that, in the interest of patient safety, we should consider alternative imaging modalities when they are diagnostically slightly inferior to CT scanning.
Provide patients with specific information about the radiation exposure associated with x-ray-based imaging studies. Initially, this information can be incorporated into patient disclosure forms and perhaps ultimately as an informed consent form.
Regarding the judicious use of CT scanning, unfortunately, it may be difficult to bring about a decrease in the number of excessive medical imaging studies ordered -- but we must strive for this.
Major conflicting factors in this dilemma are that imaging studies have become the modern physical exam, and we live in a highly litigious society and clinicians feel they cannot afford to miss anything, no matter how unlikely.[20] My answer to the first issue is that although imaging has become the physical exam, MRI can be used in place of CT for many indications, especially in younger patients.[17,21-24] The vast majority of diagnoses that CT can make, MRI can make as well or better. To appreciate the full extent of the great range of diseases that are demonstrable on MRI of the abdomen, pelvis, and chest (the regions of the body most concerning for radiation risk), the reader is referred to a recently published textbook, Abdominal Pelvic MRI, Second Edition.[25] I have edited this book.
Regarding litigation, I am personally most concerned about future class action suits regarding excessive and deleterious use of radiation from CT, from patients who were not informed of the risks.
Reduce Radiation Dose
Here, a lot of credit must be given to ongoing work by all the major manufacturers and a number of dedicated scientists and radiologists, especially pediatric radiologists, who have collectively changed machinery and protocols so pediatric patients receive considerably less radiation doses from CT scans than they had received even a few years ago. This is essentially the expression of the radiology principle of "as low as reasonably achievable" (ALARA). Currently, a great deal of work is ongoing on reducing radiation exposure in CT scans even further.
Use Alternative Imaging Modalities
My response is very short but entails a lot of work: read Abdominal Pelvic MRI, Second Edition. [25] This book describes how to perform studies (for example, it is essential to have set protocols) and how to interpret them, giving numerous examples of virtually every disease entity in the abdomen and pelvis, and provides the first chapter on MRI of the chest, in which MRI can be considered to generate diagnostically accurate and reproducible information. More ultrasound studies should be performed, especially in such settings as following up abnormalities detected on CT scans, for example, some kidney lesions.
Tell Patients About Risks
Regarding patient information, we should also inform patients of the salient points of the BEIR VII report. It may also be reasonable to mention that there is some uncertainty since the data on low-dose radiation exposure (essentially only 1 CT and lesser radiation dose exams) is not from direct x-ray exposure studies, but extrapolation from radiation exposure from atomic bomb survivors. However, these data appear to be comparable. I think that a 1 in 1000 chance of developing cancer from undergoing a single CT of 1 region of the chest, abdomen, and pelvis should be mentioned.
SOLUTIONS FOR KEY HEALTHCARE STAKEHOLDERS
I will conclude with specific recommendations to various groups:
Patients
I believe it is your right to know that radiation exposure from medical x-rays, in particular procedures utilizing high x-ray doses (eg, CT, PET, PET-CT), may result in cancer, and it is your right to request an alternative procedure when that alternative procedure generates comparable diagnostic information. Providers should know which alternative imaging modalities provide comparable information for the medical indication that you have. It is your right, based on the Hippocratic oath that all physicians have taken, that you undergo the safest test that has sufficient diagnostic accuracy to evaluate your condition. I recommend that you refer your provider to the BEIR VII report regarding radiation hazards,[1] and Abdominal Pelvic MRI [25] regarding how to perform and interpret MRI studies -- if the capabilities of MRI are questioned. Liver exams are one study in particular that should almost always be done with MRI.
RADIOLOGISTS
Referring clinicians should be educated on the hazards of radiation exposure, and discouraged from ordering studies that may pose particular health risks to patients.[13,17,24] These include CT examinations that are renal mass protocol multiphase studies, multiphase liver studies,[24] and pulmonary embolism studies in young females with a low probability for pulmonary embolism.[17] In general, extreme judicious use of CT in pediatric patients[20] and in adult patients, up to age 40, should be exercised. In adults, pelvic CT studies and chest CT studies should be held to a minimum in females, due to the risk to the gonads and fetus and the breast tissue, respectively.[17] Because of the generally long latency period for cancer development, performing CT scans in elderly patients does not carry with it the same prospects for patient injury -- so from a patient benefit perspective, in these patients, CT is not as concerning as in younger individuals. The fact that image quality is generally more consistent with CT in noncooperative patients, because it does not require the same extent of motionless attention as MRI, less hesitancy with CT is recommended in patients over age 65.
MRI studies should be subject to protocol as laid out in Abdominal Pelvic MRI,[25] dynamic gadolinium injection should be used in the great majority of patients, images should look as they do in that textbook, and images should be uniformly consistent and of high quality in cooperative patients. Good training in MRI is mandatory. The combination of diagnostic accuracy and patient safety, with equal weighting, should be our focus in all the work that we do.
Patient disclosure of radiation risk for x-ray-based modalities should be adopted, and there should be consideration of a patient informed consent form that describes the risks of radiation, and that there are alternative imaging modalities. Consideration should also be made of methods to keep track of the number and type of x-ray type procedure, to establish limits.
REFERRING HEALTHCARE PROVIDERS
I recommend that all healthcare providers become familiar with the concept that 1 in 1000 CT studies of the chest, abdomen, or pelvis may result in cancer.
Judicious ordering of CT scans and increased ordering of MRI studies, especially at centers with expertise in MRI, are warranted. On a positive note, there are many centers that perform excellent-quality body MRI. Pursue third-party payers when they deny MRI studies and recommend CT studies. They should also be apprised of BEIR VII (the executive summary is sufficient).[1]. Third-party payers should also be aware of the seminal papers that show superiority of MRI over CT in the detection of disease in the abdomen and pelvis.[21-24] The radiology facility that you refer patients to should be operating state-of-the-art equipment, with state-of-the art protocols, and should be interpreted by radiologists who have expertise in MRI. The studies should be performed, with slight variation, as outlined in Abdominal Pelvic MRI,[25] and the images should look approximately the same as those illustrated in that text.
RADIATION SCIENTISTS
Continued research into the safety aspects of various radiation-based modalities is needed. Work into mammography, digital mammography, PET, and PET/CT are necessary. Radiation exposure estimates must also be determined for the various types of CT equipment. Standard radiation dose assessments are based on single section CT, and therefore dose estimates for the variety of spiral and multidetector CTs are necessary. Estimates should be made of the risk for additive factors, such as multiple CT scans, multi-pass CT scans, and determination of whether certain time intervals are especially deleterious for inducing genetic damage and whether other time intervals lessen the additive deleterious effects of multiple CT scans.
MANUFACTURERS
Renew your work in dramatically decreasing radiation dose, and tailored decreased dose for particular studies. Machines should be equipped with warning devices when a certain radiation exposure is achieved. If all major appliances can be sold with labels that describe power usage, all CT and other high-radiation devices (PET, PET/CT) should be sold with labels that describe radiation exposure per standard procedure (for example, 2 mRad per abdomen CT). Manufacturers should also have a department of safety, whose task it is to educate users and consumers on how to manage radiation exposures to maximize ALARA, including the use of other modalities.
HOSPITALS
Incorporated within the office of patient safety should be a comprehensive office that deals with patient safety and information. Radiation is likely a much more important concern for the health of patients than HIPAA, and these should be grouped together. As part of obtaining privileges, or renewing privileges, hospital staff should take a short course on radiation safety based on the information in the BEIR VII report. CT scans, especially repeat CT scans, should be strongly discouraged in pediatric patients,[20] as should chest CT scans in young females.[17]
THIRD-PARTY PAYERS, PHARMACEUTICAL COMPANIES, AND INSURANCE COMPANIES
The most definitive scientific report has been issued that describes a 1 in 1000 chance of developing cancer with the performance of a single CT scan of the abdomen, chest, or pelvis.[1] Patients should not have procedures denied, such as MRI, because of the perception that CT is less expensive, or because CT is called for in a certain research protocol. MRI often is as diagnostically accurate as CT, if not more so,[20-24] and in circumstances such as following disease in the chest, MRI is a sufficiently accurate modality to follow masses in the chest previously discovered on CT.[25] Denying MRI in favor of CT because CT is $50 or $100 less expensive is morally inexcusable. It is reasonable to insist that radiology facilities are able to perform state-of-the-art MRI, interpreted by well-trained radiologists.
LEGISLATORS
Controls should be set as to how much radiation should be delivered to patients. It should be required that new equipment sold should have description of radiation exposure per standard exam, so that consumers (hospitals, radiologists, possibly even patients) can compare exposure between vendors and machines. If labels can be on major appliances, and thiamine content can be on a cereal box label, surely the most lethal of these agents, x-rays, can be placed on a CT scanner. Existing equipment should also have exposure rates determined. This likely means the adoption of a standardized phantom for use in these calculations. Consideration should be given to ways to keep track of patient lifetime radiation exposure - perhaps not unlike what is done with radiation workers.
MEDICAL RESEARCH FUNDING AGENCIES
Harm from x-rays may be the single largest medical issue in the healthcare continuum. Specific funding should be awarded to investigators,[2,14-16] without an extensive application process, who are already conducting radiation risk studies, to do large multi-institutional research into long-term surveys of patients who have received multiple CT studies in case-controlled studies.
REFERENCES
Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII-Phase 2. 2005. Available at: http://books.nap.edu/catalog/11340.html. Accessed February 1, 2006.
Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289-296.
Brenner DJ. Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr Radiol. 2002;32:228-223.
Ulrich H. Incidence of leukemia in radiologists. N Engl J Med. 1946;234:742-743.
Lewis EB. Leukemia and ionizing radiation. Science. 1957;125:965-972.
Bross ID. The primary principle [letter]. Environ Health Perspect. 1977;21:329-331.
Brenner DJ, Hall EJ. Risk of cancer from diagnostic x-rays. Lancet 2004;363:2192-2193.
Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A. 2003;100:13761-13766.
de Gonzalez A, Darby S. Risk of cancer from diagnostic x-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345-351.
Linton OW, Mettler FA Jr. National Council on Radiation Protection and Measurements. National conference on dose reduction in CT, with an emphasis on pediatric patients. AJR Am J Roentgenol. 2003;181:321-329.
Brenner DJ, Elliston CD. Radiation risks of body CT: what to tell our patients and other questions. Radiology. 2005;234:968-970.
Cohen BL. Cancer risk from low-level radiation. AJR Am J Roentgenol. 2002;179:1137-1143.
Brenner DJ. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology. 2004; 231:440-445.
Brenner DJ, Ron E, Staab E, et al. Helical CT and cancer risk. Pediatr Radiol. 2002;32:242-244.
Heyes GJ, Mill AJ. The neoplastic transformation potential of mammography x-rays and atomic bomb spectrum radiation. Radiat Res. 2004;162:120-127.
Millikan RC, Player JS, deCotret AR, Tse CK, Keku T. Polymorphisms in DNA repair genes, medical exposure ionizing radiation, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005;14:2326-2334.
Parker MS, Hui FK, Camacho MA, Chung JK, Broga DW, Sethi NN. Female breast radiation exposure during CT pulmonary angiography. AJR Am J Roentgenol. 2005;185:1228-1233.
UNSCEAR 2000 Medical Radiation Exposures. United Nations Scientific Committee on the Effects of Atomic Radiation Report to the General Assembly. Available at: http://cnts.wpi.edu/RSH/Docs/UN-Chernobyl/index.html. Accessed February 1, 2006.
National Council on Radiation Protection and Measurements (NCRP) Report 136. Evaluation of the Linear-Nonthreshold Dose-Response Model for Ionizing Radiation. 2001. Available at: http://www.ncrponline.org/rpt136.html Accessed February 1, 2006.
Donnelly LF. Reducing radiation dose associated with pediatric CT by decreasing unnecessary examinations. AJR Am J Roentgenol. 2005;184:655-657.
Low RN, Semelka RC, Worawattanakul S, Alzate GD, Sigeti JS. Extrahepatic abdominal imaging in patients with malignancy: comparison of MR imaging and helical CT, with subsequent surgical correlation. Radiology. 1999;210:625-632.
Low RN, Semelka RC, Worawattanakul S, Alzate GD. Extrahepatic abdominal imaging in patients with malignancy: comparison of MR imaging and helical CT in 164 patients. J Magn Reson Imaging. 2000;12:269-277.
Birchard KR, Semelka RC, Hyslop WB, et al. Suspected pancreatic cancer: evaluation by dynamic gadolinium-enhanced 3D gradient-echo MRI. AJR Am J Roentgenol. 2005;185:700-703.
Semelka RC, Martin DR, Balci C, Lance T. Focal liver lesions: comparison of dual-phase CT and multisequence multiplanar MR imaging including dynamic gadolinium enhancement. J Magn Reson Imaging. 2001;13:397-401.
Semelka RC. Abdominal-Pelvic MRI, Second Edition. Hoboken, NJ: Wiley-Liss; 2006.